Malaria.
Publié le 06/12/2021

Extrait du document
Ci-dessous un extrait traitant le sujet : Malaria.. Ce document contient 1659 mots. Pour le télécharger en entier, envoyez-nous un de vos documents grâce à notre système d’échange gratuit de ressources numériques ou achetez-le pour la modique somme d’un euro symbolique. Cette aide totalement rédigée en format pdf sera utile aux lycéens ou étudiants ayant un devoir à réaliser ou une leçon à approfondir en : Echange
Malaria.
I
INTRODUCTION
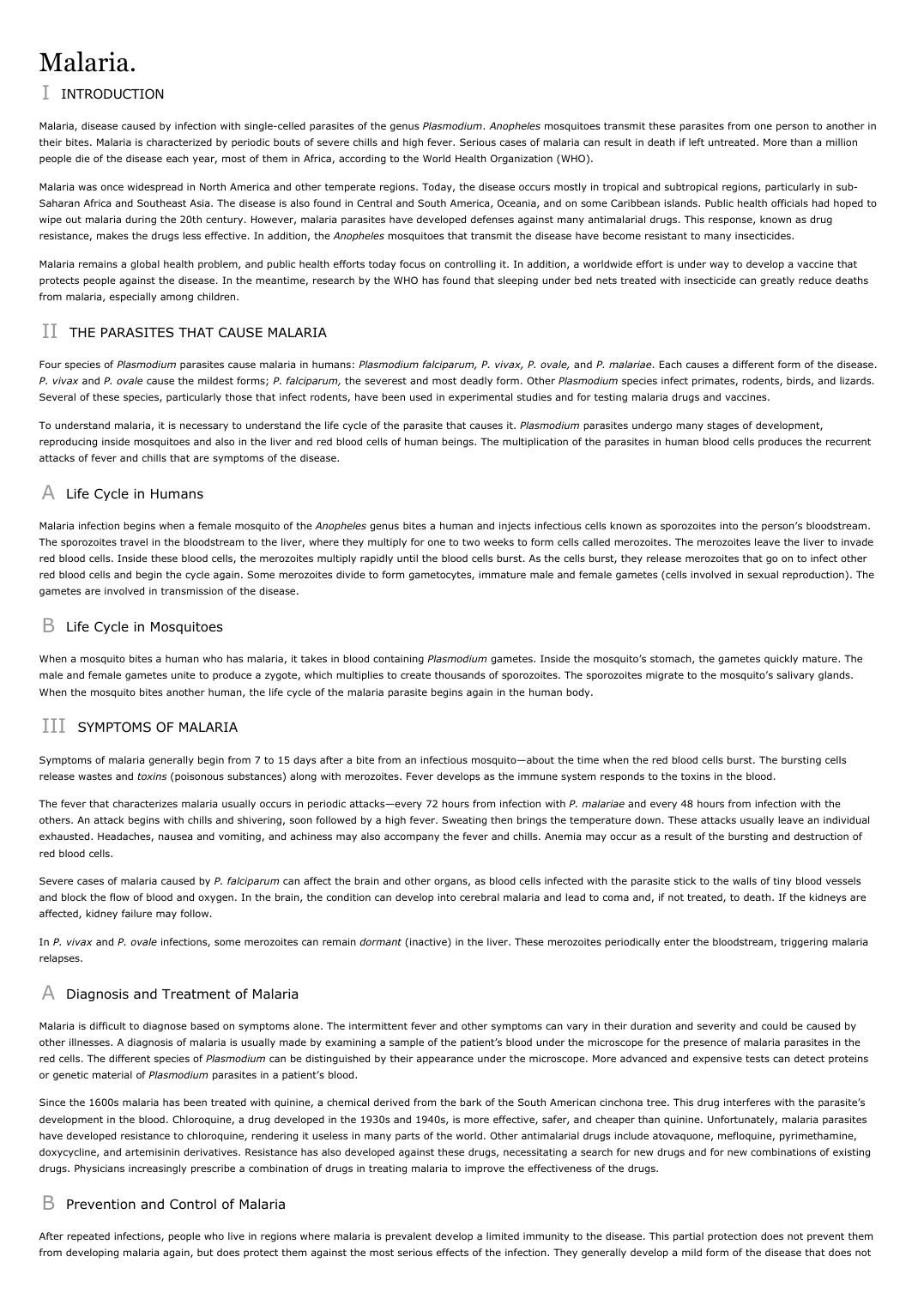
Malaria, disease caused by infection with single-celled parasites of the genus Plasmodium. Anopheles mosquitoes transmit these parasites from one person to another in
their bites. Malaria is characterized by periodic bouts of severe chills and high fever. Serious cases of malaria can result in death if left untreated. More than a million
people die of the disease each year, most of them in Africa, according to the World Health Organization (WHO).
Malaria was once widespread in North America and other temperate regions. Today, the disease occurs mostly in tropical and subtropical regions, particularly in subSaharan Africa and Southeast Asia. The disease is also found in Central and South America, Oceania, and on some Caribbean islands. Public health officials had hoped to
wipe out malaria during the 20th century. However, malaria parasites have developed defenses against many antimalarial drugs. This response, known as drug
resistance, makes the drugs less effective. In addition, the Anopheles mosquitoes that transmit the disease have become resistant to many insecticides.
Malaria remains a global health problem, and public health efforts today focus on controlling it. In addition, a worldwide effort is under way to develop a vaccine that
protects people against the disease. In the meantime, research by the WHO has found that sleeping under bed nets treated with insecticide can greatly reduce deaths
from malaria, especially among children.
II
THE PARASITES THAT CAUSE MALARIA
Four species of Plasmodium parasites cause malaria in humans: Plasmodium falciparum, P. vivax, P. ovale, and P. malariae. Each causes a different form of the disease.
P. vivax and P. ovale cause the mildest forms; P. falciparum, the severest and most deadly form. Other Plasmodium species infect primates, rodents, birds, and lizards.
Several of these species, particularly those that infect rodents, have been used in experimental studies and for testing malaria drugs and vaccines.
To understand malaria, it is necessary to understand the life cycle of the parasite that causes it. Plasmodium parasites undergo many stages of development,
reproducing inside mosquitoes and also in the liver and red blood cells of human beings. The multiplication of the parasites in human blood cells produces the recurrent
attacks of fever and chills that are symptoms of the disease.
A
Life Cycle in Humans
Malaria infection begins when a female mosquito of the Anopheles genus bites a human and injects infectious cells known as sporozoites into the person's bloodstream.
The sporozoites travel in the bloodstream to the liver, where they multiply for one to two weeks to form cells called merozoites. The merozoites leave the liver to invade
red blood cells. Inside these blood cells, the merozoites multiply rapidly until the blood cells burst. As the cells burst, they release merozoites that go on to infect other
red blood cells and begin the cycle again. Some merozoites divide to form gametocytes, immature male and female gametes (cells involved in sexual reproduction). The
gametes are involved in transmission of the disease.
B
Life Cycle in Mosquitoes
When a mosquito bites a human who has malaria, it takes in blood containing Plasmodium gametes. Inside the mosquito's stomach, the gametes quickly mature. The
male and female gametes unite to produce a zygote, which multiplies to create thousands of sporozoites. The sporozoites migrate to the mosquito's salivary glands.
When the mosquito bites another human, the life cycle of the malaria parasite begins again in the human body.
III
SYMPTOMS OF MALARIA
Symptoms of malaria generally begin from 7 to 15 days after a bite from an infectious mosquito--about the time when the red blood cells burst. The bursting cells
release wastes and toxins (poisonous substances) along with merozoites. Fever develops as the immune system responds to the toxins in the blood.
The fever that characterizes malaria usually occurs in periodic attacks--every 72 hours from infection with P. malariae and every 48 hours from infection with the
others. An attack begins with chills and shivering, soon followed by a high fever. Sweating then brings the temperature down. These attacks usually leave an individual
exhausted. Headaches, nausea and vomiting, and achiness may also accompany the fever and chills. Anemia may occur as a result of the bursting and destruction of
red blood cells.
Severe cases of malaria caused by P. falciparum can affect the brain and other organs, as blood cells infected with the parasite stick to the walls of tiny blood vessels
and block the flow of blood and oxygen. In the brain, the condition can develop into cerebral malaria and lead to coma and, if not treated, to death. If the kidneys are
affected, kidney failure may follow.
In P. vivax and P. ovale infections, some merozoites can remain dormant (inactive) in the liver. These merozoites periodically enter the bloodstream, triggering malaria
relapses.
A
Diagnosis and Treatment of Malaria
Malaria is difficult to diagnose based on symptoms alone. The intermittent fever and other symptoms can vary in their duration and severity and could be caused by
other illnesses. A diagnosis of malaria is usually made by examining a sample of the patient's blood under the microscope for the presence of malaria parasites in the
red cells. The different species of Plasmodium can be distinguished by their appearance under the microscope. More advanced and expensive tests can detect proteins
or genetic material of Plasmodium parasites in a patient's blood.
Since the 1600s malaria has been treated with quinine, a chemical derived from the bark of the South American cinchona tree. This drug interferes with the parasite's
development in the blood. Chloroquine, a drug developed in the 1930s and 1940s, is more effective, safer, and cheaper than quinine. Unfortunately, malaria parasites
have developed resistance to chloroquine, rendering it useless in many parts of the world. Other antimalarial drugs include atovaquone, mefloquine, pyrimethamine,
doxycycline, and artemisinin derivatives. Resistance has also developed against these drugs, necessitating a search for new drugs and for new combinations of existing
drugs. Physicians increasingly prescribe a combination of drugs in treating malaria to improve the effectiveness of the drugs.
B
Prevention and Control of Malaria
After repeated infections, people who live in regions where malaria is prevalent develop a limited immunity to the disease. This partial protection does not prevent them
from developing malaria again, but does protect them against the most serious effects of the infection. They generally develop a mild form of the disease that does not
last long and is unlikely to be fatal. Infants and children are especially vulnerable to malaria because they have not yet built up immunity to the parasite. Some people
have genetic traits that help them resist malaria. Sickle-cell anemia and thalassemia, for example, are inherited blood disorders linked to malaria resistance.
Travelers who lack immunity to malaria should take precautionary measures when visiting areas where the disease is prevalent. Such measures include using insect
repellents, wearing protective clothing that covers the skin, and sleeping under mosquito nets. Antimalarial drugs are also available as a preventive measure. However,
these drugs have some serious side effects and are not suitable for everyone.
B1
Vaccine Research
Currently, no effective vaccine against malaria exists, although researchers around the world are working to develop one. Such a vaccine would either stop the infection
from developing or from becoming severe or else prevent transmission of the infection. Vaccine researchers are targeting different stages in the parasite's life cycle,
hoping to block the liver stage, to interfere with reproduction in the blood cells, or to halt transmission to the mosquito. They are also investigating the possibility of
incorporating genes for malaria antigens (substances that stimulate the production of disease-fighting antibodies) into vaccines.
Developing a malaria vaccine has been difficult because the Plasmodium parasite has hundreds of different strategies for evading the human immune system. Many of
these strategies are not well understood, and it is difficult to develop a vaccine that will block all of the parasite's ways of getting past the immune system. A successful
vaccine will need to target several stages of the parasite's life cycle. Progress toward a vaccine has also been slow because the parasite is difficult to produce and study
in the laboratory, as it must live inside the cells of another organism.
Testing of several potential vaccines in humans was under way in the 2000s. A vaccine known as RTS,S was given to children between the ages of one and four and was
found to protect against infection 45 percent of the time during an 18-month observation period.
B2
Antimosquito Measures
In the absence of an effective vaccine and with the rise of drug resistance, malaria prevention has had to rely on basic antimosquito measures. Such measures include
draining sites where mosquitoes lay their eggs, covering water channels, and introducing into ponds fish that feed on mosquito larvae.
The United States virtually eradicated malaria in the late 1940s and early 1950s through the use of the insecticide DDT. However, DDT was later banned in the United
States and many other countries because of its harmful effects on the environment. Moreover, many species of Anopheles mosquitoes are now resistant to a wide range
of insecticides, including DDT, as a result of the widespread use of these chemicals. Newer insecticides are effective but are also much more expensive and must be
used carefully. Controlled spraying of the inside of houses is effective where the mosquitoes have not developed resistance.
Insecticide-treated bed nets have proven to be one of the most effective malaria prevention strategies. The World Health Organization distributed bed nets to families
with children under age 5 in several African countries and found that the death rate from malaria dropped by 50 to 60 percent among children in these countries. One
problem with treated bed nets has been that they lose their effectiveness over time. Newer nets, however, retain their effectiveness for several years. Although the
nets are inexpensive, even their modest cost is beyond the means of many families in developing countries.
Microsoft ® Encarta ® 2009. © 1993-2008 Microsoft Corporation. All rights reserved.
Malaria.
I
INTRODUCTION
Malaria, disease caused by infection with single-celled parasites of the genus Plasmodium. Anopheles mosquitoes transmit these parasites from one person to another in
their bites. Malaria is characterized by periodic bouts of severe chills and high fever. Serious cases of malaria can result in death if left untreated. More than a million
people die of the disease each year, most of them in Africa, according to the World Health Organization (WHO).
Malaria was once widespread in North America and other temperate regions. Today, the disease occurs mostly in tropical and subtropical regions, particularly in subSaharan Africa and Southeast Asia. The disease is also found in Central and South America, Oceania, and on some Caribbean islands. Public health officials had hoped to
wipe out malaria during the 20th century. However, malaria parasites have developed defenses against many antimalarial drugs. This response, known as drug
resistance, makes the drugs less effective. In addition, the Anopheles mosquitoes that transmit the disease have become resistant to many insecticides.
Malaria remains a global health problem, and public health efforts today focus on controlling it. In addition, a worldwide effort is under way to develop a vaccine that
protects people against the disease. In the meantime, research by the WHO has found that sleeping under bed nets treated with insecticide can greatly reduce deaths
from malaria, especially among children.
II
THE PARASITES THAT CAUSE MALARIA
Four species of Plasmodium parasites cause malaria in humans: Plasmodium falciparum, P. vivax, P. ovale, and P. malariae. Each causes a different form of the disease.
P. vivax and P. ovale cause the mildest forms; P. falciparum, the severest and most deadly form. Other Plasmodium species infect primates, rodents, birds, and lizards.
Several of these species, particularly those that infect rodents, have been used in experimental studies and for testing malaria drugs and vaccines.
To understand malaria, it is necessary to understand the life cycle of the parasite that causes it. Plasmodium parasites undergo many stages of development,
reproducing inside mosquitoes and also in the liver and red blood cells of human beings. The multiplication of the parasites in human blood cells produces the recurrent
attacks of fever and chills that are symptoms of the disease.
A
Life Cycle in Humans
Malaria infection begins when a female mosquito of the Anopheles genus bites a human and injects infectious cells known as sporozoites into the person's bloodstream.
The sporozoites travel in the bloodstream to the liver, where they multiply for one to two weeks to form cells called merozoites. The merozoites leave the liver to invade
red blood cells. Inside these blood cells, the merozoites multiply rapidly until the blood cells burst. As the cells burst, they release merozoites that go on to infect other
red blood cells and begin the cycle again. Some merozoites divide to form gametocytes, immature male and female gametes (cells involved in sexual reproduction). The
gametes are involved in transmission of the disease.
B
Life Cycle in Mosquitoes
When a mosquito bites a human who has malaria, it takes in blood containing Plasmodium gametes. Inside the mosquito's stomach, the gametes quickly mature. The
male and female gametes unite to produce a zygote, which multiplies to create thousands of sporozoites. The sporozoites migrate to the mosquito's salivary glands.
When the mosquito bites another human, the life cycle of the malaria parasite begins again in the human body.
III
SYMPTOMS OF MALARIA
Symptoms of malaria generally begin from 7 to 15 days after a bite from an infectious mosquito--about the time when the red blood cells burst. The bursting cells
release wastes and toxins (poisonous substances) along with merozoites. Fever develops as the immune system responds to the toxins in the blood.
The fever that characterizes malaria usually occurs in periodic attacks--every 72 hours from infection with P. malariae and every 48 hours from infection with the
others. An attack begins with chills and shivering, soon followed by a high fever. Sweating then brings the temperature down. These attacks usually leave an individual
exhausted. Headaches, nausea and vomiting, and achiness may also accompany the fever and chills. Anemia may occur as a result of the bursting and destruction of
red blood cells.
Severe cases of malaria caused by P. falciparum can affect the brain and other organs, as blood cells infected with the parasite stick to the walls of tiny blood vessels
and block the flow of blood and oxygen. In the brain, the condition can develop into cerebral malaria and lead to coma and, if not treated, to death. If the kidneys are
affected, kidney failure may follow.
In P. vivax and P. ovale infections, some merozoites can remain dormant (inactive) in the liver. These merozoites periodically enter the bloodstream, triggering malaria
relapses.
A
Diagnosis and Treatment of Malaria
Malaria is difficult to diagnose based on symptoms alone. The intermittent fever and other symptoms can vary in their duration and severity and could be caused by
other illnesses. A diagnosis of malaria is usually made by examining a sample of the patient's blood under the microscope for the presence of malaria parasites in the
red cells. The different species of Plasmodium can be distinguished by their appearance under the microscope. More advanced and expensive tests can detect proteins
or genetic material of Plasmodium parasites in a patient's blood.
Since the 1600s malaria has been treated with quinine, a chemical derived from the bark of the South American cinchona tree. This drug interferes with the parasite's
development in the blood. Chloroquine, a drug developed in the 1930s and 1940s, is more effective, safer, and cheaper than quinine. Unfortunately, malaria parasites
have developed resistance to chloroquine, rendering it useless in many parts of the world. Other antimalarial drugs include atovaquone, mefloquine, pyrimethamine,
doxycycline, and artemisinin derivatives. Resistance has also developed against these drugs, necessitating a search for new drugs and for new combinations of existing
drugs. Physicians increasingly prescribe a combination of drugs in treating malaria to improve the effectiveness of the drugs.
B
Prevention and Control of Malaria
After repeated infections, people who live in regions where malaria is prevalent develop a limited immunity to the disease. This partial protection does not prevent them
from developing malaria again, but does protect them against the most serious effects of the infection. They generally develop a mild form of the disease that does not
last long and is unlikely to be fatal. Infants and children are especially vulnerable to malaria because they have not yet built up immunity to the parasite. Some people
have genetic traits that help them resist malaria. Sickle-cell anemia and thalassemia, for example, are inherited blood disorders linked to malaria resistance.
Travelers who lack immunity to malaria should take precautionary measures when visiting areas where the disease is prevalent. Such measures include using insect
repellents, wearing protective clothing that covers the skin, and sleeping under mosquito nets. Antimalarial drugs are also available as a preventive measure. However,
these drugs have some serious side effects and are not suitable for everyone.
B1
Vaccine Research
Currently, no effective vaccine against malaria exists, although researchers around the world are working to develop one. Such a vaccine would either stop the infection
from developing or from becoming severe or else prevent transmission of the infection. Vaccine researchers are targeting different stages in the parasite's life cycle,
hoping to block the liver stage, to interfere with reproduction in the blood cells, or to halt transmission to the mosquito. They are also investigating the possibility of
incorporating genes for malaria antigens (substances that stimulate the production of disease-fighting antibodies) into vaccines.
Developing a malaria vaccine has been difficult because the Plasmodium parasite has hundreds of different strategies for evading the human immune system. Many of
these strategies are not well understood, and it is difficult to develop a vaccine that will block all of the parasite's ways of getting past the immune system. A successful
vaccine will need to target several stages of the parasite's life cycle. Progress toward a vaccine has also been slow because the parasite is difficult to produce and study
in the laboratory, as it must live inside the cells of another organism.
Testing of several potential vaccines in humans was under way in the 2000s. A vaccine known as RTS,S was given to children between the ages of one and four and was
found to protect against infection 45 percent of the time during an 18-month observation period.
B2
Antimosquito Measures
In the absence of an effective vaccine and with the rise of drug resistance, malaria prevention has had to rely on basic antimosquito measures. Such measures include
draining sites where mosquitoes lay their eggs, covering water channels, and introducing into ponds fish that feed on mosquito larvae.
The United States virtually eradicated malaria in the late 1940s and early 1950s through the use of the insecticide DDT. However, DDT was later banned in the United
States and many other countries because of its harmful effects on the environment. Moreover, many species of Anopheles mosquitoes are now resistant to a wide range
of insecticides, including DDT, as a result of the widespread use of these chemicals. Newer insecticides are effective but are also much more expensive and must be
used carefully. Controlled spraying of the inside of houses is effective where the mosquitoes have not developed resistance.
Insecticide-treated bed nets have proven to be one of the most effective malaria prevention strategies. The World Health Organization distributed bed nets to families
with children under age 5 in several African countries and found that the death rate from malaria dropped by 50 to 60 percent among children in these countries. One
problem with treated bed nets has been that they lose their effectiveness over time. Newer nets, however, retain their effectiveness for several years. Although the
nets are inexpensive, even their modest cost is beyond the means of many families in developing countries.
Microsoft ® Encarta ® 2009. © 1993-2008 Microsoft Corporation. All rights reserved.
↓↓↓ APERÇU DU DOCUMENT ↓↓↓
Liens utiles
- Présentation de la Malaria
- Ronald Ross1857-1932Pathologiste et médecin militaire, qui étudia (1897) le rôle du moustique dans latransmission de la malaria.
- Anophèle:Le moustique responsable de la malaria.
- Malaria